(CHRONIC OBSTRUCTIVE PULMONARY DISEASE)
*This information is taken from the links at the bottom of this page and is provided to you as an educational service. It is not meant to be a substitute for consulting with your own physician.
What is COPD?
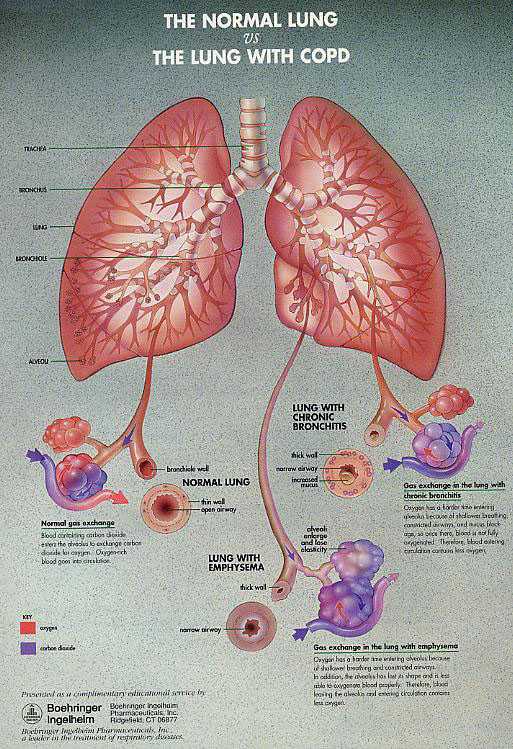
Chronic obstructive pulmonary disease (COPD) is an umbrella term used to describe airflow obstruction that is associated mainly with emphysema and chronic bronchitis.
Emphysema causes irreversible lung damage by weakening and breaking the air sacs within the lungs. As a result, elasticity of the lung tissue is lost, causing airways to collapse and obstruction of airflow to occur.
Chronic Bronchitis is an inflammatory disease that begins in the smaller airways within the lungs and gradually advances to larger airways. It increases mucus in the airways and increases bacterial infections in the bronchial tubes, which, in turn, impedes airflow.
How prevalent is COPD?
The exact prevalence of COPD is not well defined, yet it affects tens of millions of Americans and is a serious health problem in the U.S.:
In 1994, it was estimated that 16 million patients have been diagnosed with some form of COPD and as many as 16 million more are undiagnosed.
New government data based on a 1998 prevalence survey suggest that three million Americans have been diagnosed with emphysema and nine million are affected by chronic bronchitis.
COPD is the fourth leading cause of death
in the U.S. in 1998.
COPD accounted for 112,584 deaths in 1998.
COPD accounted for an estimated 668,362
hospital discharges in 1998.
What are the risk factors for COPD?
Long-term smoking is the most frequent cause of COPD. It accounts for 80 to 90 percent of all cases. A smoker is 10 times more likely than a non-smoker to die of COPD.
Other risk factors include:
Heredity
Second-hand smoke
Exposure to air pollution at work and in
the environment
A history of childhood respiratory infections
What are the symptoms of COPD?
The symptoms of COPD include: chronic cough, chest tightness, shortness of breath, an increased effort to breathe, increased mucus production, and frequent clearing of the throat.
How does COPD have an impact on a patient's life?
COPD decreases the lungs' ability to take
in oxygen and remove carbon dioxide. As the
disease progresses, the walls of the lungs'
small airways and alveoli lose their elasticity. The
airway walls collapse, closing off some
of the smaller air passages and narrowing larger ones.
The passageways become clogged with mucus.
Air continues to reach the alveoli when the lungs
expand during inhalation; however, it is
often unable to escape during exhalation because the air passages tend
to collapse during exhalation, trapping the "stale" air in the lungs.
A typical course of COPD might begin after
a person has been smoking for 10 years, during
which symptoms are usually not very noticeable.
Then the patient begins developing a
productive, chronic cough. Usually, after
age 40, the patient may begin developing shortness
of breath during exertion, which continues
and worsens over time.
Though the severity may vary, COPD patients
have some degree of airway obstruction. While symptoms may vary over time,
the patient will notice a gradual deterioration over the course
of four to five years. Repeated and increased
productive coughing begins to disable patients,
who over time take longer to recover from
these attacks.
Many patients with severe COPD-related lung
damage have so much difficulty breathing
when lying down that they sleep in a semi-sitting
up position. For COPD patients, the
combination of too little oxygen and too
much carbon dioxide in the blood may also have an impact on the brain, and can cause a variety
of other health problems, including headache, sleeplessness, impaired mental ability and
irritability.5
The clinical development of COPD is typically described in three stages, as defined by the American Thoracic Society:
Stage 1: Lung function (as measured by FEV1 or forced expiratory volume in one second) is greater than or equal to 50 percent of predicted normal lung function. There is minimal impact on health-related quality of life. Symptoms may progress during this stage, and patients may begin to experience severe breathlessness, requiring evaluation by a pulmonologist.
Stage 2: FEV1
lung function is 35 to 49 percent of predicted normal lung function, and
there is a significant impact on health-related
quality of life.
Stage 3: FEV1 lung function is less than 35 percent of predicted normal lung function, and there is a profound impact on health-related quality of life.
What can COPD patients do to help themselves live as normal a life as possible?
The best weapon against COPD is prevention: avoiding or ceasing smoking. Avoiding smoking almost always prevents COPD from developing, and ceasing smoking slows the disease process.
Pulmonary rehabilitation programs and medical treatment can be useful for certain patients with COPD. The key goal should be to improve physical endurance in order to overcome the conditions
that cause shortness of breath and limit capacity for physical exercise and daily activities.
What are the goals of COPD care?
It is important to identify and treat COPD at the earliest time possible in its natural history. Unfortunately, the diagnosis of COPD is frequently made when patients are in their late 50s or 60s, when FEV1 has declined to a symptomatic range, and when quality of life is rapidly deteriorating. Therefore, the goal of any physician treating patients with COPD is to help relieve their patients' symptoms, to help patients better manage the effects of their disease and to live as full and active lives as possible.
If patients work closely with physicians to develop a complete respiratory care program, they can:
Improve lung function
Reduce hospitalizations
Prevent acute episodes
Minimize disability
Delay early death
What are the key components of COPD care?
In addition to smoking cessation, depending upon the severity of the disease, treatments may include bronchodilators that open up air passages in the lungs, antibiotics, and exercise to strengthen muscles. People with COPD may eventually require supplemental oxygen and, in the end-stages of the disease, may have to rely on mechanical respiratory assistance.
1. Medications that are prescribed for people with COPD may include:
Fast-acting beta2-agonists, such as albuterol which can help to open narrowed airways
Anticholinergic bronchodilators, such as
ipratropium bromide, and
theophylline derivatives, all of which help
to open narrowed airways.
Long-acting bronchodilators, which help relieve constriction of the airways and help to prevent bronchospasm associated with COPD.
Inhaled or oral corticosteroids, which help reduce inflammation. Currently, the role of these anti-inflammatory medications in COPD therapy is not well defined, and they are not yet indicated for COPD in the U.S. However, clinical trials are underway.
Antibiotics, which are often given at the first sign of a respiratory infection to prevent further damage and infection in diseased lungs.
Expectorants, which help loosen and expel mucus secretions from the airways, and may help make breathing easier.
In addition, other medications may be prescribed to manage conditions associated with COPD.
These may include:
Diuretics, which are given as therapy to avoid excess water retention associated with right-heart failure, which may occur in some COPD patients.
Digitalis (usually in the form of digoxin), which strengthens the force of the heartbeat. It is used with caution in COPD patients, especially if their blood oxygen tensions are low, since they become vulnerable to arrhythmia when taking this drug.
Painkillers, cough suppressants, and sleeping pills, which should be used only with caution, because they depress breathing to some extent.
2. People with COPD can better manage their disease by:
Avoiding:
Cigarettes, dust, air pollution, cigarette
smoke, and work-related fumes
Contact with people who have respiratory
infections, such as colds and flu
Excessive heat, cold or high altitudes
Maintaining:
A healthy diet and an exercise program supervised
by a health care provider
Regular contact and visits with a health
care provider so that he or she can
carefully monitor the disease; this includes
having regular spirometry tests
3. Additional treatment options for patients with COPD may include:
Regular immunizations, such as for flu and
pneumococcal pneumonia
Pulmonary rehabilitation, which can improve
exercise tolerance
The use of supplemental oxygen, especially
in patients in the later stages of COPD
Bullectomy, or surgical removal of large
air spaces in the lungs
Lung volume reduction surgery, which is
currently considered experimental
Lung transplantation, which also has proven
effective in some end-stage COPD patients
RECOGNIZING SIGNS AND SYMPTOMS
OF CHRONIC OBSTRUCTIVE PULMONARY
DISEASE
Recognizing changes in signs and symptoms of Chronic Obstructive Pulmonary Disease (COPD) is an important part of managing your illness. Knowing when symptoms are changing is helpful so that treatment and other interventions can begin promptly. Early treatment is most effective. If sever symptoms are present, it is vital to begin the appropriate treatment immediately. Accurate and timely assessment of your symptoms can help you and your health care provider decide if treatment should begin in the home, at your health care provider's office or in the emergency room.
Early symptoms or warning signs are unique to each person. These warning signs may be the same, similar or entirely different with each episode. Usually you will be the best person to know if you are having difficulty breathing. However, some changes are more likely to be noticed by other persons, so it is important to share this information sheet with your family and those close to you.
A change or increase in the symptoms you usually experience may be the only early warning sign. You may notice one or more of the following:
-an increase or decrease in the amount of sputum produced
-an increase in the thickness or stickiness of sputum
-a change in sputum color to yellow or green or the presence of blood in the sputum
-an increase in the severity of shortness of breath, cough and/or wheezing
-a general feeling of ill health
-ankle swelling
-forgetfulness, confusion, slurring of speech and sleepiness
-difficulty sleeping
-using more pillows or sleeping in a chair instead of a bed to avoid shortness of breath
-an unexplained increase or decrease in
weight
-increased feeling of fatigue and lack of energy that continues
-a lack of sexual drive
-increasing morning headaches, dizzy spells, restlessness
Symptoms do not go away when they are ignored. Therefore, knowing when to call your health care provider is very important in managing your chronic lung disease. It is very important for you to work with your health care provider to determine the appropriate treatment for signs and symptoms of COPD.
WHEN TO CALL THE DOCTOR
Call immediately if disorientation, confusion, slurring of speech or sleepiness occurs during an acute respiratory infection.
Call within 6-8 hours if shortness of breath or wheezing does not stop or decrease with inhaled bronchodilator treatments one hour apart.
Call within 24 hours if you notice one or more of the following severe respiratory symptoms:
- change in color, thickness, odor or amount of sputum persists
- ankle swelling lasts even after a night of sleeping with your feet up
- you awaken short of breath more than once a night
- fatigue lasts more than one day
Severe respiratory symptoms are a life-threatening emergency. Have an action plan for getting emergency care quickly in the event of severe symptoms. Inform family members and those who are close to you of this emergency action plan.
It is very important to work with your health care provider to determine the appropriate treatment steps for signs and symptoms of respiratory difficulty. These are guidelines and your specific treatment plan should be determined by you and your health care provider.
While there are many effective measures you can do at home to treat signs and symptoms, there are also actions that should be avoided. If you do any of the following, it can make your condition worse:
Do not take any extra doses of theophylline
Do not take codeine or any other cough suppressant
Do not use over-the-counter nasal sprays for more than 3 days
Do not increase the liter flow of prescribed oxygen
Do not smoke
Do not wait any longer than 24 hours to
contact your doctor if symptoms continue
We learn early in life that food and air are basic to our survival. They are so basic, in fact, that to describe the importance of eating and breathing seems unnecessary--too simplistic for words.
For people with chronic obstructive pulmonary disease, eating should be treated as importantly as breathing and should not be taken for granted. A well-nourished body helps the COPD patient to fight infections, and it may help prevent illness and cut down on hospitalizations.
Food is fuel, and the body needs fuel for all of its activities, including breathing. Because the COPD patient expends much energy in the simple act of breathing, his ventilatory muscles can require up to ten times the calories required by a healthy person's muscles. This is why it is so important for persons with COPD to eat properly. Good nutritional support helps maintain the ventilatory functions of the lungs, while improper nutrition can cause wasting of the diaphragm and other pulmonary muscles.
The American Association for Respiratory Care has gathered some nutrition tips for persons with COPD. These are general guidelines only; your physician is your best source of information on diet and other information about your lung disease.
1. Eat foods from each of the basic food groups: fruits and vegetables, dairy products, cereal and grains, proteins.
2. Limit your salt intake. Too much sodium can cause you to retain fluids that may interfere with breathing.
3. Limit your intake of caffeinated drinks. Caffeine may interfere with some of your medications and may also make you feel nervous.
4. Avoid foods that produce gas or make you feel bloated. The best process to use in eliminating foods from your diet is trial and error.
5. Try to eat your main meal early. This way, you will have lots of energy to carry you through the day.
6. Choose foods that are easy to prepare. Don't waste all of your energy preparing a meal. Try to rest before eating so that you can enjoy your meal.
7. Avoid foods that supply little or no nutritional value.
8.Try eating six small meals a day instead of three large ones. This will keep you from filling up your stomach and causing shortness of breath.
9. If you are using oxygen, be sure to wear your cannula while eating - and after meals, too. Eating and digestion require energy, and this causes your body to use more oxygen.
10.Try to eat in a relaxed atmosphere, and make your meals attractive and enjoyable.
11. Consult your physician if you have other dietary restrictions, such as ulcers, or if you are overweight or underweight.
12. In many states, there are agencies that will provide meals for people for a small fee or at no charge. Check with local church organizations or government agencies to see what is available in your area.
A proper diet will not cure your disease, but it will make you feel better. You will have more energy, and your body will be able to fight infection better. These tips from the American Association for Respiratory Care are general guidelines. Your own physician is your best source of specific information. Good nutrition and a balanced diet are essential to everyone's health, but patients with lung disease must be even more careful than most about following good nutrition guidelines.
MEDLINE PLUS
http://www.nlm.nih.gov/medlineplus/copdchronicobstructivepulmonarydisease.html
COPD ALERT
http://www.geocities.com/wrozenba/COPD.html
American Lung Association® - Fact Sheet
http://www.lungusa.org/diseases/copd_factsheet.html
American Lung Association® - Around the Clock with COPD
http://www.lungusa.org/diseases/copd_clock.html
